A leading New Zealand mental health research foundation has rebranded and is targeting a portion of its funding towards anxiety and depression research as it works to meet the rising need for mental health research in New Zealand.
Over the past 57 years the Whau Mental Health Research Foundation, previously known as the Oakley Mental Health Research Foundation, has invested around $2.5 million in almost 200 research projects addressing a wide range of mental health issues in New Zealand.
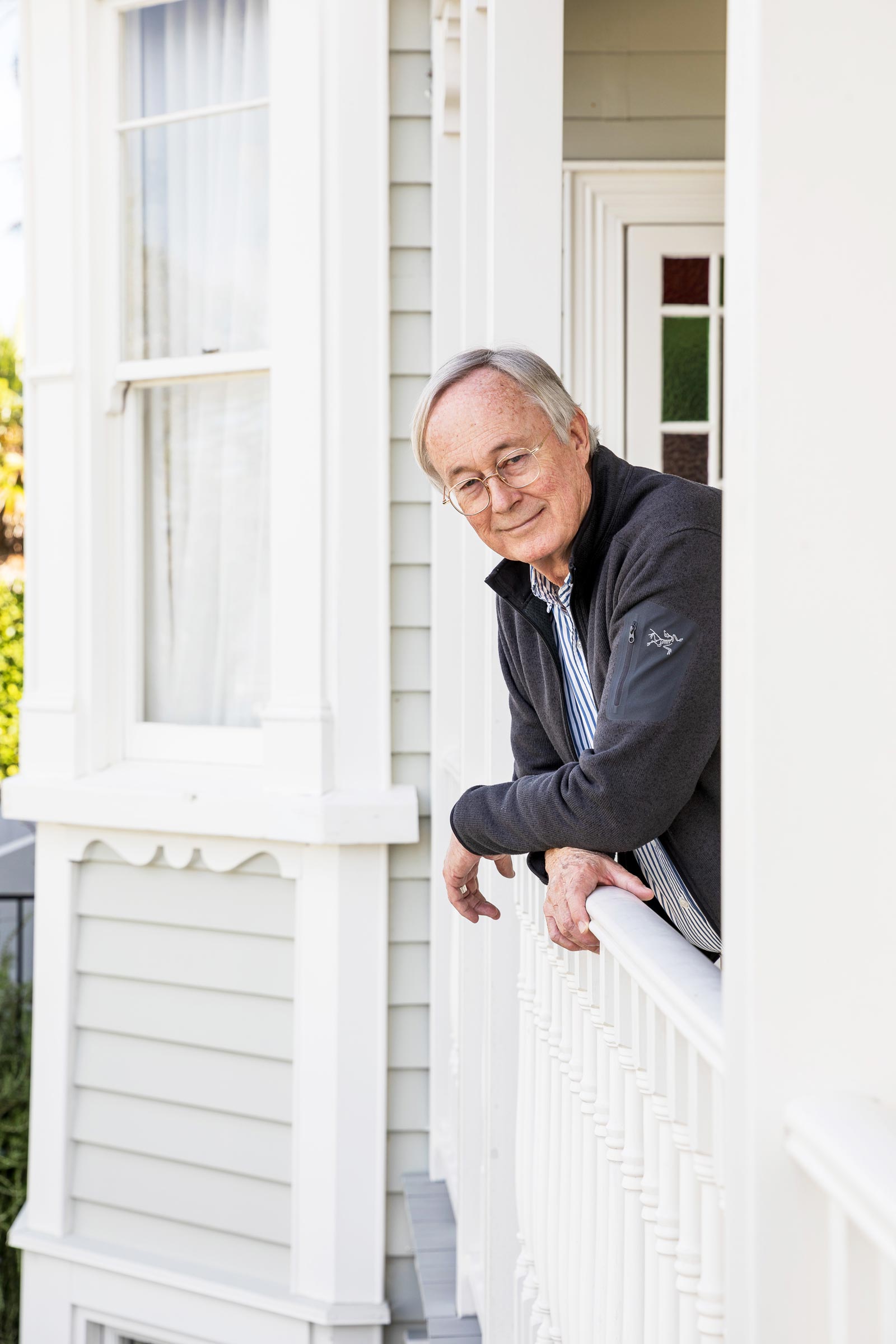
Chairman Robert Kydd says in 2025, alongside the foundation’s usual support for a broad range of mental health projects, there will be a targeted fund dedicated to anxiety and depression research, with a strong emphasis on addressing these challenges among young people.
“This fund will support studies working to understand the factors that contribute to these conditions, as well as exploring effective treatments and interventions to improve mental health outcomes,” said Kydd.
“Many organisations from academic institutions to NGOs are conducting impactful work in these areas and we aim to strengthen their capacity through strategic funding and a commitment to rigorous evaluation. By empowering these groups to deliver meaningful, evidence-based results, we contribute to building a stronger, more effective mental health landscape in Aotearoa.”
Kydd says the need for impactful mental health research has never been greater, with nearly half of New Zealanders experiencing mental illness or distress during their lifetime.
“New Zealand is facing a mental health crisis, with rising rates of mental illness and suicide, particularly among young people,” said Kydd.
“We have one of the highest youth suicide rates in the OECD, with Māori and Pasifika youth disproportionately affected. Mental distress is on the rise, with one in five young people aged 15 – 24 reporting high levels of psychological distress, according to the 2022/2023 New Zealand Health Survey. Mental health services are struggling to cope, with long wait times and staff shortages across the country.
“The COVID-19 pandemic has further exacerbated these issues, increasing feelings of isolation, financial stress and anxiety. Despite a $1.9 billion investment in mental health by the government in 2019, progress in expanding services and addressing these challenges has been slow, leaving many in urgent need of care.”
Kydd says the Whau Foundation is committed to meeting this need by expanding its fund, growing public support, and fostering strategic partnerships with like-minded organisations and corporate sponsors.
“The Whau Foundation helps to address gaps in knowledge and service delivery by funding innovative research. Our work focuses on evidence-based practices and developing effective interventions.
“We prioritise finding out what actually works in mental health care, ensuring that our initiatives are grounded in research and real-world outcomes. Through advancing understanding in the field, we aim to alleviate pressure on the healthcare system and offer better support to those in need.”
Previous grants from the Whau Foundation have led to significant scientific and clinical outcomes, supporting both emerging and established researchers in their pursuit of innovative solutions to mental health challenges.
Recent projects which received funding from the Foundation include Dr Karolina Stasiak’s computerised Cognitive Behaviour Therapy (cCBT), which developed new generation e-therapy for young people with mild to moderate depression. The research served as a prototype for SPARX – a video game that teaches young people CBT techniques for dealing with symptoms of depression.
The Foundation also contributed to research by Dr Rose Crossin which explored the negative effects of alcohol on New Zealander’s mental health.
Whau Foundation research grants for 2024 / 2025 include:
- Morgan Blind (University of Waikato): Project SOLVE and rangatahi in Aotearoa: Co-designing and evaluating a digital single-session intervention for adolescent mental health in New Zealand.
- Jai Whelan (University of Otago): Exploring Methamphetamine Treatment Options, Harm Reduction and Stigma in Aotearoa.
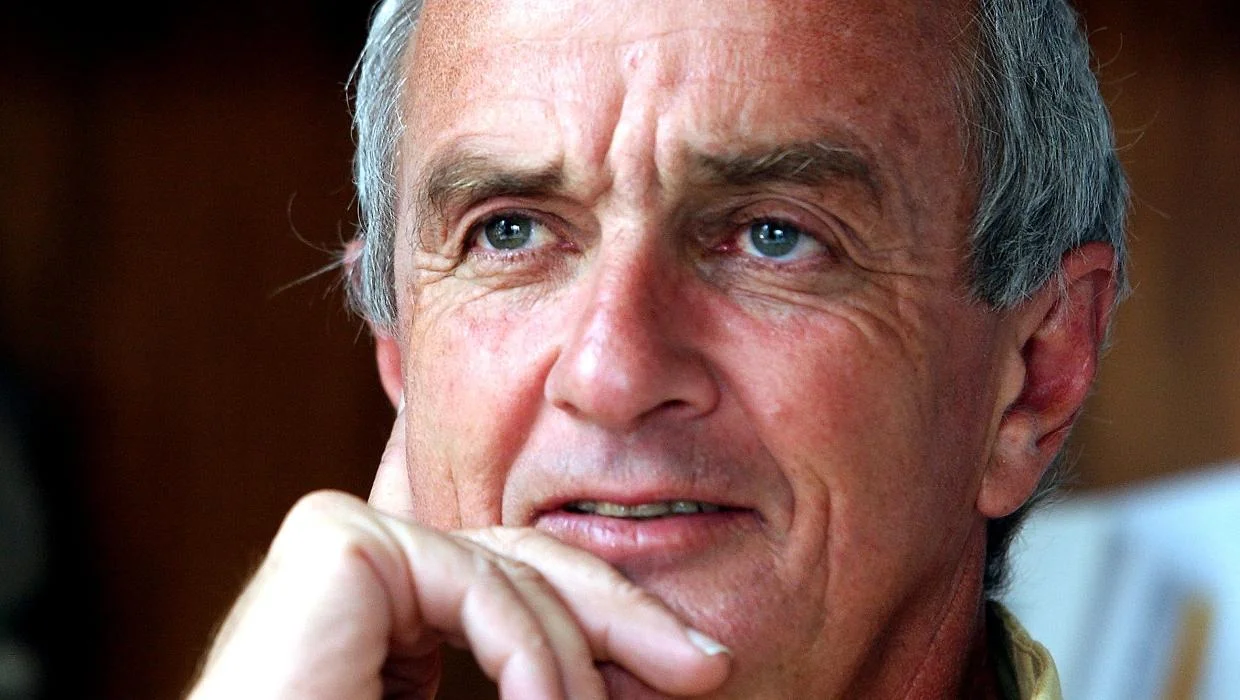
- Professor Bruce Arroll (Auckland City Mission/Calder Clinic): Written Exposure therapy: Effective, Briefer, Evidence-based treatment for PTSD conducted by a wider range of clinicians.
- Professor Dirk De Ridder (University of Otago): A triple network stimulation approach for the treatment of internalising psychopathology.
About Whau Foundation:
The Whau Foundation is dedicated to funding high-quality mental health research that enhances evidence-based knowledge, increases research capacity, and improves health outcomes, well-being, and equity for all New Zealanders.
Over the past 57 years, the Foundation has invested approximately $2.5 million in over 180 research projects, addressing a wide range of mental health issues. These grants have led to significant scientific and clinical outcomes, supporting both emerging and established researchers in their pursuit of innovative solutions to mental health challenges.
Named after the Whau tree, the New Zealand native that provides shelter for other species of plants to grow and thrive, the Foundation aims to nurture ground-breaking discoveries and advancements in the mental health field.
For more information and interview requests please contact:
Lewis Hampton
Payper Co-Founder
lewis@payper.co